Biofilms and Recurrent UTIs
Urinary tract infections (UTIs) are among the most common bacterial infections affecting millions worldwide each year. Between 50% and 60% of women will experience at least one urinary tract infection (UTI) in their life. 30-44% of females with an initial UTI will experience a second UTI [1]. With each UTI, the risk of another UTI increases. Recurrent UTIs are defined as having at least two infections in six months or three in a year. While these recurrent UTIs seem to happen independently of one another, they are often caused by bacteria from an initial infection that was never fully cleared. Bacteria can survive antibiotic treatment and the immune system by staying protected by a biofilm. These bacteria eventually end their dormancy, grow their populations, and cause recurrent UTIs.
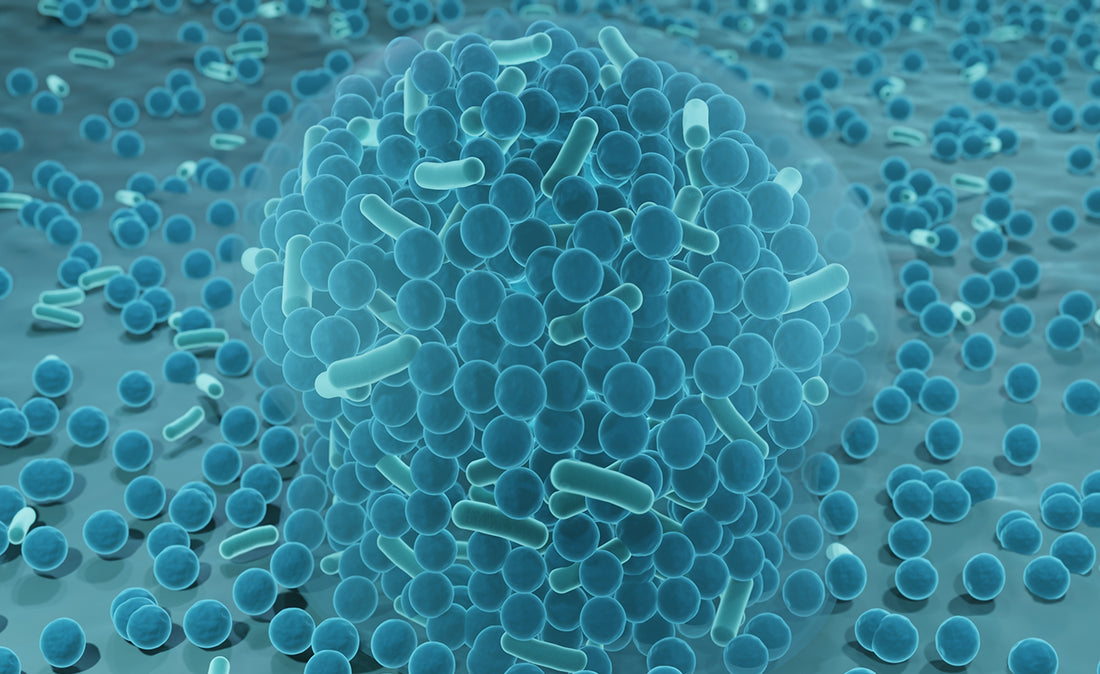
What are Biofilms?
Biofilms are closed bacterial communities encased within a matrix of extracellular polymeric substances (EPS), which they produce. This matrix acts as a protective shield, allowing bacteria within the biofilm to adhere to urinary tract surfaces such as the bladder lining or urinary catheters. These biofilm communities can lay dormant and eventually cause relapse infections. While the bacteria are contained within their shield, the body is less likely to mount an effective response to their presence. Biofilms are difficult to detect, and urine cultures may also come up negative. When bacteria are periodically released or escape from the biofilm, the body recognizes a threat. This triggers an inflammatory response, heightening symptoms of a UTI. This can be experienced as a cycle of acute symptoms, followed by periods of fewer or no symptoms. This cycle can continue, causing recurrent UTIs.
Biofilm formation is considered one of the most important mechanisms behind the high rates of recurrence and antimicrobial resistance that are often associated with UTIs. Once established, biofilms are notoriously difficult to eradicate with standard antibiotic treatments. Biofilm formation significantly alters the behavior and resilience of bacteria in the urinary tract. Bacteria within biofilms exhibit enhanced resistance to antibiotics, up to 1,000 times more compared to planktonic (free-floating) bacteria [2]. This resistance is partly due to limited antibiotic penetration through the EPS matrix and altered bacterial physiology within the biofilm structure.
Cleanse and Help Prevent Biofilm Formation
Maintaining a clean urinary tract is crucial in preventing the formation of biofilms and recurrent UTIs. Biofilms are particularly challenging because they provide bacteria with enhanced resistance to antibiotics, making infections harder to treat and more likely to recur. By regularly cleansing the urinary tract, you can help flush out bacteria before they have a chance to form biofilms, thereby reducing the risk of chronic infections. Simple practices like staying hydrated, urinating frequently, and incorporating targeted supplements can be effective strategies in supporting urinary health and preventing biofilm-related complications.
Learn how UT-Fem® products can help protect you against biofilms and recurrent UTIs. Stay ahead of recurrent UTIs with our fast-acting urinary tract flush and daily defense.*
➜ Explore our products and discover the difference that proactive care can make in your life.
References:
- Kramer, Melissa. Chronic urinary tract infection vs recurrent UTI. Live UTI Free. August, 2020.
- Rasmussen TB, Givskov M. Int J Med Microbiol. 2006;296(2–3):149–161.
 You’re Getting FREE SHIPPING!
You’re Getting FREE SHIPPING!
 Your Order Comes With a Money - Back Guarantee
Your Order Comes With a Money - Back Guarantee